The ethics of changing genes in the embryo
From the moment we began to unlock the secrets of the genome, the complete set of DNA including all genes and understand the effects that genes can have on human health, the idea of modifying the human genome – and hence controlling these effects – has held both promise and peril. Visions of a bright future free from the sufferings of genetic disease contrast starkly with darker fears of a genetically-engineered ‘Brave New World’.
Until recently, however, human germline genetic modification, changes to the genome that will be passed down to future generations, was more the stuff of speculation than scientific endeavour. Existing techniques for germline genetic modification were too inefficient, imprecise and impractical to justify their use in human beings; whatever we might think of modifying the genome in principle, the risks and technical hurdles were simply too great to attempt such experiments in practice. With the advent of so-called ‘gene editing’ technologies such as the CRISPR/Cas9 system, however, this has changed. The possibility of (relatively) precise and effective methods that could make, for the first time, targeted human germline genetic modification a serious prospect, has prompted the international scientific and ethical community to revisit and re-evaluate these issues. In particular, research published by a group of Chinese scientists in April 2015 that used gene editing to modify human embryos has reignited a heated ethical debate over whether the use of these techniques in humans, and especially in human embryos, ought to be permitted.
Modifying the human genome: sacredness, naturalness and human dignity
Before considering the case of embryo gene editing, we should ask: is there anything inherently wrong with genetic modification?
Some might argue that the ‘sanctity of the human genome’ provides us with an upfront reason against human genetic modification.
"We should ask: is there anything inherently wrong with genetic modification?"
Yet although a certain popular mystique may attach to the idea of genetics, there is nothing sacred or sacrosanct about the genome as such. The human genome – the genome of humanity as a whole, and the unique individual genome we each possess – is merely the product of our evolutionary history to date, the result of both happy and unhappy accidents of nature. Although particular techniques may present specific safety concerns, somatic genetic modification (that will not be inherited by offspring) should be considered on a par with other interventions we might choose to make to our own bodies: medical treatment, changes in diet and lifestyle, or cosmetic changes such as dyeing one’s hair or getting a suntan.
Likewise, arguments that genetic modification is ‘unnatural’ or essentially against human dignity appear to fetishise the human genome to an unreasonable extent. In the world of modern medicine and skyscrapers, the idea that we should reject all things ‘unnatural’ seems unconvincing, if not downright implausible. And what is it about the genome in its exact present state that confers ‘dignity’? We do not consider existing variation in the sequences of individual human genomes to be a threat to dignity; nor should deliberately inducing a genetic change be considered as such.
The effects of genetic changes themselves, of course, may have consequences for dignity. One might think, however, that being forced to endure the effects of genetic disease that could potentially be prevented by genetic modification is likely to be more of an insult to dignity than being cured! Although full clinical application of genome editing is still some way off, vague concerns about dignity ought not to impede us from pursuing the potential for therapeutic goals that this technology might offer.
Embryo ethics
If human genetic research and changes to the human genome sequence are in themselves nothing to worry about, why then did the Chinese study cause such a furore? The answer, of course, is that it involved the use of human embryos.
Opinions on the moral status of the human embryo remain deeply divided. For those who believe that the embryo has equivalent moral status to a grown human person, research involving the use or destruction of human embryos is likely to be unacceptable, or acceptable only in a limited range of circumstances. Yet this was not at the heart of the objections raised over this study. Many scientists and many jurisdictions accept human embryo research, notably in the context of stem cells; the issue in this case was not the use of embryos in general, but their use in this particular type of research.
So, why might genome editing research on human embryos be seen as particularly problematic? One possible response might be that embryos cannot decide for themselves whether to undergo genome editing – they are unable to give consent, and have no choice over the alterations inflicted upon them. But this holds true for all forms of embryo research: embryos at the pre-14 day stage are simply incapable of giving consent or exercising any form of choice.
"So, why might genome editing research on human embryos be seen as particularly problematic?"
Those who accept the use of embryos in stem cell research generally accept that, lacking any form of sentience, self-awareness or self-will (indeed, lacking any kind of neurological structure that would form a basis for such characteristics, since at this stage embryos are simply composed of largely undifferentiated cells) embryos are not the kinds of beings for whom consent and choice are relevant concepts. It seems clear that the widespread concerns over this research were not primarily based on any moral status or rights that embryos might have.
Germline genome editing: research versus reproduction
At the heart of the matter, then, is the fact that the use of genome editing in human embryos constitutes what many were quick to call “germline modification”. These words for some raise the spectre of coercive eugenics and associated ideas of state-mandated population genetic engineering as a form of social control – morally unacceptable for a host of reasons, first and foremost the disproportionate infringement of liberty and personal autonomy that such a regime would entail. But such a dystopian vision bears no relation to the research that was actually carried out in the embryo gene editing study.
In fact, I suggest that what we are actually ethically concerned about when we talk of ‘germline modification’ is the creation of genetically modified children, and the introduction of genetic changes that may be inherited by future generations. In the context of the Chinese study, such concerns are entirely misplaced. The embryos used in the research were never destined to be implanted; indeed, even had they been implanted, they were ‘non-viable’, generated in such a way that they could never have developed to full term. No genetically modified babies could have been created by this procedure, nor could the modifications have been passed on to any descendants.
"for ethical purposes the relevant distinction should be between research and reproduction"
Instead of worrying about ‘germline modification’, therefore, for ethical purposes the relevant distinction should be between research and reproduction: not whether embryos are modified, but whether the modified embryos are used in research or implanted for reproduction. This is not to say that genome editing for reproductive purposes will never be morally justifiable; indeed, as the technology becomes better-understood and its potential therapeutic uses explored, there may be very good moral reasons to pursue it, not least the prevention of disease and suffering. But if reproductive uses are what we want to avoid, at least while the technology is still in its experimental stages, then regulation should focus on preventing these specific uses, not on preventing embryo genome editing altogether.
Non-viable embryos: a red herring
The use of non-viable embryos in the Chinese study was intended to address moral concerns, but made the research scientifically problematic: the biological differences between these and viable embryos throw into question the validity of the results obtained in relation to normal embryos. Moreover, it failed to solve any of the moral problems associated with embryo genome editing research.
If one believes that the human embryo has some sort of intrinsic moral value, the fact that an embryo is unable to survive past a certain point does not necessarily overcome the moral problems associated with its use and destruction – any more than deliberately creating a child with a fatal inherited disease would legitimise taking that child at birth and using it in research on the grounds that it would not survive to adulthood.
If, on the other hand, the concern were to prevent the birth of genetically modified children, then regulating which embryos can be implanted, rather than which embryos can be used in research, would be a more appropriate solution. While some might see the use of non-viable embryos as an additional safeguard, a law stating that only non-viable embryos may be used in genome editing research would be as subject to wilful violation as a law stating that any embryos (viable or non-viable) so used should not be implanted. In either case, effective enforcement will be required.
Risk and responsibility
As noted, in the past the risks associated with genetic modification technologies have provided one of the most salient arguments against the procedure. The new genome editing techniques that have been developed, although vastly more accurate and efficient, are still not without some element of uncertainty. Any potential clinical application will certainly need to take into account the levels of risk that might be involved in the use of genome editing procedures, and more scientific work will undoubtedly be needed to define what the risks are and how they can be managed, before proceeding to its use as a treatment.
"In thinking about embryo gene editing research, however, the question is: risk to whom?"
In thinking about embryo gene editing research, however, the question is: risk to whom? If no embryos are implanted and no children are born, no persons (either mothers or children) will be put at risk of harm by genome editing. On the other hand, if we refuse to explore promising research avenues because of misplaced concerns about risk, people who might have been helped by the development of these technologies will suffer as a result of our failure to act. An ethical approach to risk requires us to evaluate the possible consequences both of action and of inaction, and to realise that we are responsible for harms caused by the latter as well as the former. In this case the opportunity costs of not pursuing genome editing research are likely to be significant, given the potential of this research eventually to produce new treatments.
Furthermore, without research we will not be able to undertake the rigorous scientific evaluation of risks and uncertainties that is precisely what is required in order to move towards eventual safe application. In other words, if we do not pursue this research because we think its uses as a treatment are too risky at this stage, we are ensuring that they will forever remain too risky for want of proper investigation! A ban on research is certainly not the answer.
Further information
- EuroStemCell article about the science behind the the CRISPR/Cas9 technology that can be used to efficiently edit genes
- EuroStemCell article about the ethics of using embryos in research
- UK scientists apply for licence to edit genes in human embryos
- Article written from a US perspective about genetic modification of embyros
- Details about the work published by scientists from Sun Yat-zen University showing they had successfully modified (non-viable) human embryos
- TED talk by Harvey Fineberg about evolution of the human species including the use of genetic modification
Acknowledgements
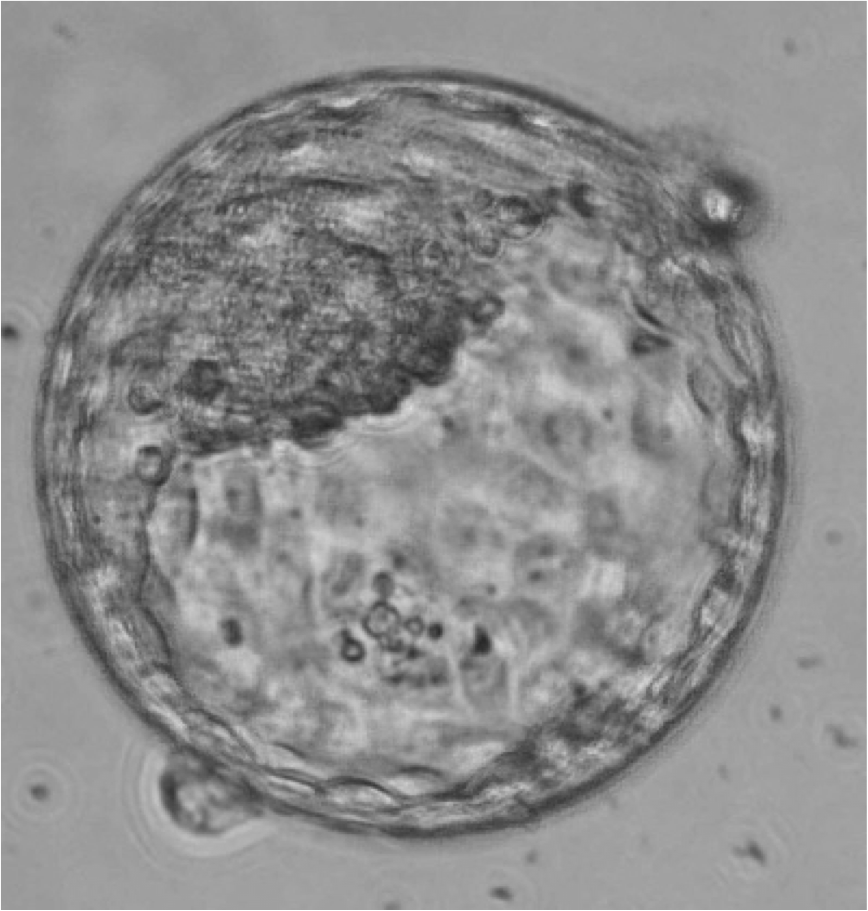
This article was written by Sarah Chan, University of Edinburgh. Image Credit: Human blastocyst aged 6 days. Jenny Nichols, University of Cambridge.
Updated by: Sarah Chan