Medicine and Stem Cells
In our Medicine and Stem Cells section you can explore the conditions and diseases that can be treated with stem cell therapy or help inform your participation in clinical trials or treatment.

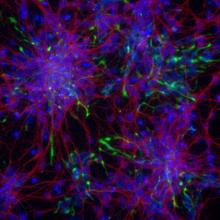
Cerebral Palsy: how could stem cells help?
• EuroStemCell resource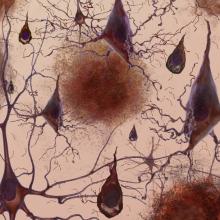
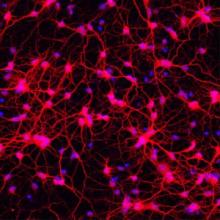
Alzheimer’s disease: how could stem cells help?
• EuroStemCell resource