Reproduction and Fertility: How could stem cells help?
HOW COULD STEM CELLS BE USED TO MAKE EGGS AND SPERM?
For many who are unable to have a biological child, due to the absence of or faulty eggs or sperm, newspaper stories about scientists making sperm or eggs from pluripotent stem cells in the lab has the potential to be a game changer. But what is the science behind these headlines and what are the limitations in moving forward? This Q&A summarizes recent developments towards treating fertility and genetic disease with eggs and sperm made from pluripotent stem cells.
WHAT ARE PLURIPOTENT STEM CELLS?
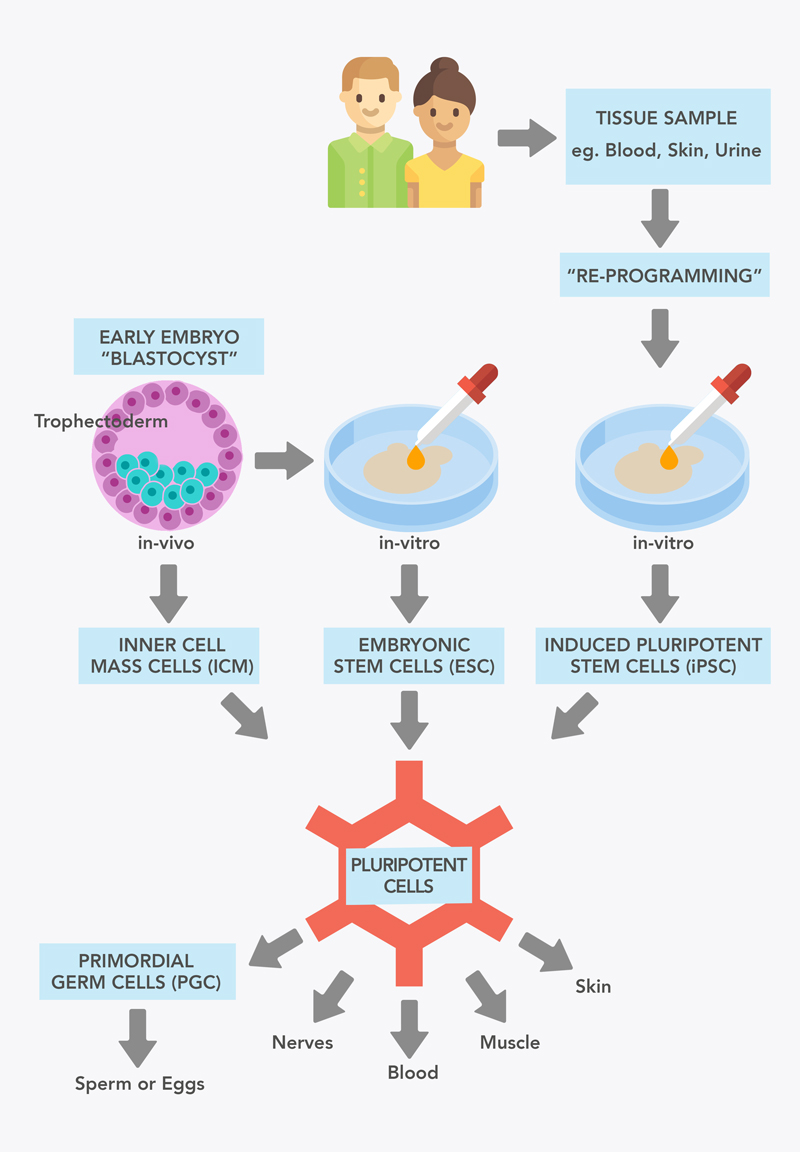
Pluripotent cells turn into all of the types of cells that make up the body from muscle, nerve, skin cells, to eggs and sperm (see Figure 1). Pluripotent cells are found as Inner Cell Mass (ICM) cells in 5 day old embryos - those used in in-vitro fertilisation (IVF), but are quickly lost when the embryo implants and develops. Pluripotent cells cannot be found in fetuses or adults. When ICM pluripotent cells are grown outside the embryo in the lab, they are known as ‘embryonic stem cells’ (ESC). ESC were the first population of pluripotent stem cells (PSC) available to researchers, first derived from human embryos in 1998.
In 2006, the Japanese researcher Shinya Yamanaka showed mouse skin cells could be made into Pluripotent Stem Cells, through a process known as ‘re-programming’. These cells resembled embryonic stem cells and were dubbed adult derived induced pluripotent stem cells (iPSC). These cells, like embryonic stem cells, have the potential to form all cell types of the body, including eggs and sperm. The generation of induced pluriportent stem cells was revolutionary to the stem cell field and medicine as a whole and was awarded the Nobel Prize in 2012 only 5 years after they were successfully made from human cells. Induced pluripotent stem cells have now been made from many cell types in addition to skin - including blood, hair follicles and cells from urine!
CAN WE MAKE EGGS AND SPERM FROM PLURIPOTENT STEM CELLS?
Yes - in mice. Eggs and sperm have not yet been made from human pluripotent stem cells (PSC). They have been made from mouse pluripotent stem cells leading to healthy, fertile pups from either PSC derived sperm or eggs.
Two researchers from Japan have pioneered this technology; Katsuhiko Hayashi and Mitinori Saitou. In 2011, they were the first to show that sperm made from male PSC enabled infertile mice to have healthy and fertile pups. They continued their research, showing the next year that female PSC could be turned into eggs that could develop to healthy and fertile pups.
While these results are very exciting there are a few things that were critical to this success….
- The starting cell type: Following embryo implantation the Inner Cell Mass turns into ‘epiblast’ cells. Some of these epiblast cells exit the developing embryo and turn into primordial germ cells (PGCs). These PGCs later migrate back into the fetus and take residence in the forming ovaries or testes, where they turn into eggs or sperm respectively. While researchers have reported production of cells similar to epiblast (Rathjen 1999, Tesar 2007, Brons 2007), Hayashi and colleagues showed that these Epiblast stem cells (Epi-SC), were not very effective at making PGCs. Instead, they developed the Epiblast-like cell (Epi-LC), a new type of epiblast cell from mouse embryonic stem cells, which more efficiently turns into PGCs and subsequently eggs or sperm.
- Cell type purity: When turning pluripotent stem cells into specific types of cells it’s difficult to get every cell to respond exactly the same. This can lead to cell types you don’t necessarily want, for example in the case of Hayashi and colleagues, cells that form tumors or cells that don’t form eggs and sperm. Purification of PGCs was critical for removing those unwanted cell types.
- A requirement for in-vivo maturation: While healthy and fertile pups were produced in both studies, the process of making functional mature eggs and sperm required transplantation to mouse ovaries or testicles respectively. Finding out how the ovary/testicle causes this maturation will be important for maturing PGCs in the lab, minimising invasive and risky procedures.
WHAT ARE THE CURRENT BARRIERS TO MAKING EGGS AND SPERM FROM HUMAN PLURIPOTENT STEM CELLS?
If eggs and sperm could be made from adult body cells, through induced pluripotent stem cell technology, the applications for individuals struggling with infertility or with the possibility of passing on genetic diseases would be extensive. Currently, there are three major barriers to applying the process used in the mice studies to humans:
Making PGCs with high efficiency and without using fetal tissues
Making sure these human PGCs make eggs and sperm but not tumours
Working out how to mature human PGCs to eggs and sperm in the lab to avoid transplanting to people - avoiding both invasive procedures and tumour risk
Recently a British human study succeeded in making PGCs with quite high efficiency, ~40% PGC-like cells, in the absence of fetal tissues. They also believe they have found a way to purify this human PGC-like population to avoid tumours. No efforts to mature or transplant these cells were reported. This study makes strides towards resolving barriers 1 and 2.
Concurrently, the mouse field is trying to work out how to mature PGCs without needing ovary/testicular tissues or transplantation (barriers 1 and 3). Healthy fertile pups have been made from sperm produced entirely in-vitro but using 2-8 day old pup testicular tissue. Similarly, Saitou and Hayashi, have shown that mouse PGC-like cells can be matured to functional eggs in-vitro, no doubt based on findings in the same institute for in-vitro maturation of PGCs.
COULD WE MAKE EGGS FROM MALE CELLS OR SPERM FROM FEMALE CELLS?
At the moment there is no evidence in mammals that sperm can be made from female cells or eggs from male cells. This is surprising considering the plethora of research available from decades of research in gamete development and sex determination. Unfortunately, the scientific understanding of this barrier since the 2011-2012 Hayashi papers is far behind the media attention created around the possibility of same-sex reproduction.
What evidence do we have for or against this being possible?
Evidence for production of eggs from XY (male) cells or sperm from XX (female) cells:
There are a couple of studies that suggest maturing Primordial Germ Cells in a mixed XX/XY environment could allow production of eggs from XY (male) cells (Ford 1975, Evans 1977). These studies however have been difficult to interpret and have not continued in the last 40 years, suggesting some part of the studies was not working as hoped. More recently there were a couple of publications that showed production of egg-like cells from male mouse pluripotent cells (Hubner 2003, Qing 2007) but in the last decade they have not shown pups from these methods, also suggesting the technology does not work. Thus at this stage there is shaky evidence for production of eggs from XY (male) cells and no evidence for production of sperm from XX (female) cells.
Evidence against production of eggs from XY (male) cells or sperm from XX (female) cells:
Decades of research into mammalian gamete formation and sex selection show that it is not possible to form eggs from cells with Y chromosome genes or sperm from cells without them (reviewed in Taketo 2015). These studies argue that production of sperm from XX (female) cells or eggs from XY (male) cells is not possible. Additionally, the barrier to the development of healthy individuals is seen in human sex chromosome disorders associated with sterility including;
- XY females - Swyer syndrome
- XX males - de la Chapelle syndrome
- XXY males - Klinefelter syndrome
- XO females - Turner syndrome
Keep in mind that most of these studies look at conditions where both the eggs/sperm and the ovaries/testes carry dysfunctional genetics. What happens if healthy XY PGCs are put in a healthy XX ovary or healthy XX PGC into a healthy teste? This experiment is yet to be performed, however can be performed using the Hayashi methods discussed above.
IS THE CREATION OF AN EMBRYO FROM SPERM AND EGG FROM THE SAME INDIVIDUAL CLONING?
No. If it becomes possible to make eggs and sperm from the same individual to produce an embryo the chances of the embryo being genetically identical to the ‘parent’ are extremely small.
Eggs and sperm made from pluripotent stem cells (PSC) would have a random mixture of chromosomes from the mother and father for a total of 23 chromosomes. Fusion of the random egg chromosomes with the random sperm chromosomes would mean statistically billions of children would need to be produced by this method produce a genetically identical baby. This is the power of chromosome mixing in the production of eggs and sperm which means your parents would need to have trillions of children to statistically end up with another you.
Cloning involves taking the genetic information from a single donor adult cell (46 chromosomes) and transplanting it into an egg that has had its genetic material removed. The resulting embryo is an exact genetic copy in every case. Cloning for reproductive purposes is banned all over the world.
HOW COULD GENETIC DISEASES BE AVOIDED WITH PLURIPOTENT STEM CELL DERIVED EGGS AND SPERM?
For couples who carry genetic disease or a child with a genetic disease, there is currently only one way to actively avoid implantation of an embryo carrying the genetic disease; Pre-Implantation Genetic Diagnosis (PGD). This process involves IVF and then removing 4-5 cells from the trophectoderm (see Figure 1), the cells that go on to form placenta, amniotic membranes etc. during pregnancy, These cells are genetically sequenced for the disease mutation and an embryo negative for the disease can then be implanted in the mother. Depending on the disease, often multiple rounds of IVF will be needed to get a healthy embryo that will lead to a baby.
It is not possible to genetically test eggs and sperm prior to fertilisation as in order to analyze the cell’s DNA with current techniques it would need to be destroyed.
Recent developments have attempted to use ‘cut and paste’ DNA modifying technology, known as CRISPR/Cas9 to edit the genetic makeup of the fertilised embryo directly (Liang 2015, Ma 2017, Fogarty 2017). Currently, this technology affects non-targeted parts of the DNA, requires many embryos and brings up many ethical issues. For these reasons it is unlikely genetic modification of embryos will ever be used over the clinical standard Pre-Implantation Genetic Diagnosis.
Producing eggs and sperm from pluripotent stem cells (PSC) will provide a powerful source of cells for genetic corrections. Their ability to grow in the lab means you have plenty of cells to check that the disease has been corrected and many more to turn into eggs and sperm. There are a few ways genetic disease could be corrected in pluripotent stem cells including;
- CRISPR/Cas9: DNA would be added or removed to fix the disease mutation. Corrected cells would be then be selected and grown - meaning all resulting eggs and sperm made from these corrected PSC would not carry the disease. Unintended mutations could also be tested for prior to production of eggs and sperm.
- For mosaic diseases (diseased that don’t affect all cells), single pluripotent stem cellss not carrying the disease could be identified and grown for egg and sperm production.
- Removal of extra chromosomes: A recent paper from Saitou has successfully removed extra chromosomes from pluripotent cells and used them to make healthy mice. They also corrected chromosome number for Down Syndrome and in Klinefelter XXY human iPSC. This could be applied to human disorders with extra chromosomes (Klinefelter, Down Syndrome, Patau Syndrome, Edward’s Syndrome) or to ‘healthy’ people who produce many eggs/sperm with sporadic addition or removal of chromosomes, happening more commonly during ageing.
These correction technologies would be unlikely to be used for averting genetic disease as the current clinical standard Pre-implantation Genetic Diagnosis is currently cheaper and more straightforward.
Acknowledgements:
The original version of this factsheet was created by Heather Main and reviewed by Megan Munsie, with expert input from Amander Clark.
Aktualisiert von: Heather Main